Adenosine Deaminase (ADA)(Pericardial fluid)
New
880₹
In stock
Hyderabad
0 Reviews
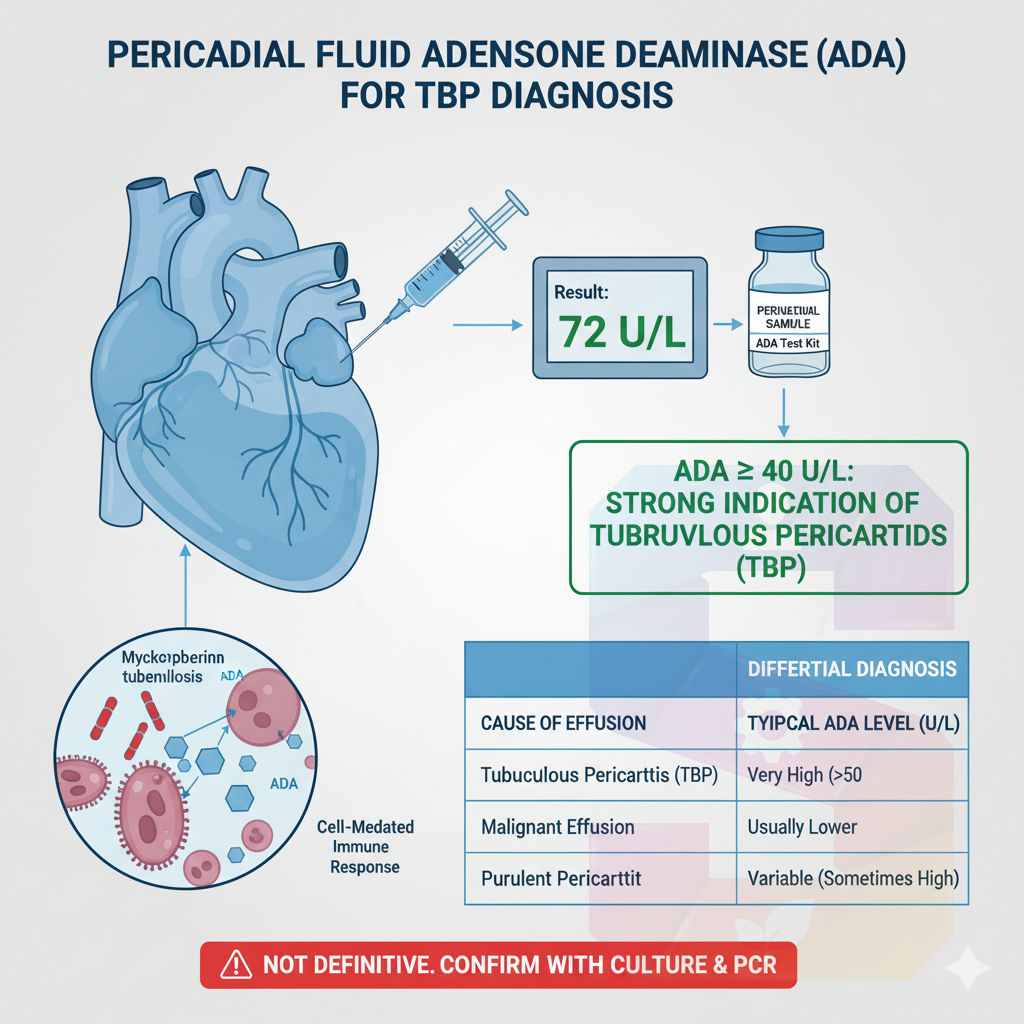
Adenosine Deaminase (ADA) activity in pericardial fluid is a highly valuable, rapid, and cost-effective biomarker used for the diagnosis of Tuberculous Pericarditis (TBP).
Key Concepts and Mechanism
Primary Role: The main utility of measuring pericardial fluid ADA is to rapidly differentiate TBP (Tuberculosis of the heart sac) from other causes of pericardial effusion (fluid around the heart), such as malignancy or non-tuberculous infections.
Source: ADA is mainly produced by T-lymphocytes and macrophages as part of the cell-mediated immune response.
TBP Pathogenesis: In TBP, the Mycobacterium tuberculosis bacteria stimulate a vigorous local immune reaction, leading to a high concentration of ADA-releasing T-lymphocytes migrating into the pericardial space.
Diagnostic Interpretation
Tuberculous Pericarditis (TBP): ADA levels are typically markedly elevated in TBP.
Cut-off Value: A commonly accepted and highly reliable cut-off value for suggesting TBP is \ge 40 \text{ U/L} (or IU/L).
Note: Some studies suggest a cut-off of \ge 50 \text{ U/L} for even higher specificity.
Performance: At the \ge 40 \text{ U/L} threshold, pericardial fluid ADA generally demonstrates high sensitivity (87-93%) and high specificity (83-97%) for diagnosing TBP.
Differential Diagnosis:
High ADA : Strongly suggests TBP.
Low ADA : Essentially rules out TBP in a patient with a low pre-test probability, but high levels can rarely be seen in purulent (bacterial) pericarditis or certain malignancies.
Key Concepts and Mechanism
Primary Role: The main utility of measuring pericardial fluid ADA is to rapidly differentiate TBP (Tuberculosis of the heart sac) from other causes of pericardial effusion (fluid around the heart), such as malignancy or non-tuberculous infections.
Source: ADA is mainly produced by T-lymphocytes and macrophages as part of the cell-mediated immune response.
TBP Pathogenesis: In TBP, the Mycobacterium tuberculosis bacteria stimulate a vigorous local immune reaction, leading to a high concentration of ADA-releasing T-lymphocytes migrating into the pericardial space.
Diagnostic Interpretation
Tuberculous Pericarditis (TBP): ADA levels are typically markedly elevated in TBP.
Cut-off Value: A commonly accepted and highly reliable cut-off value for suggesting TBP is \ge 40 \text{ U/L} (or IU/L).
Note: Some studies suggest a cut-off of \ge 50 \text{ U/L} for even higher specificity.
Performance: At the \ge 40 \text{ U/L} threshold, pericardial fluid ADA generally demonstrates high sensitivity (87-93%) and high specificity (83-97%) for diagnosing TBP.
Differential Diagnosis:
High ADA : Strongly suggests TBP.
Low ADA : Essentially rules out TBP in a patient with a low pre-test probability, but high levels can rarely be seen in purulent (bacterial) pericarditis or certain malignancies.
Adenosine Deaminase (ADA) activity in pericardial fluid is a highly valuable, rapid, and cost-effective biomarker used for the diagnosis of Tuberculous Pericarditis (TBP).
Key Concepts and Mechanism
Primary Role: The main utility of measuring pericardial fluid ADA is to rapidly differentiate TBP (Tuberculosis of the heart sac) from other causes of pericardial effusion (fluid around the heart), such as malignancy or non-tuberculous infections.
Source: ADA is mainly produced by T-lymphocytes and macrophages as part of the cell-mediated immune response.
TBP Pathogenesis: In TBP, the Mycobacterium tuberculosis bacteria stimulate a vigorous local immune reaction, leading to a high concentration of ADA-releasing T-lymphocytes migrating into the pericardial space.
Diagnostic Interpretation
Tuberculous Pericarditis (TBP): ADA levels are typically markedly elevated in TBP.
Cut-off Value: A commonly accepted and highly reliable cut-off value for suggesting TBP is \ge 40 \text{ U/L} (or IU/L).
Note: Some studies suggest a cut-off of \ge 50 \text{ U/L} for even higher specificity.
Performance: At the \ge 40 \text{ U/L} threshold, pericardial fluid ADA generally demonstrates high sensitivity (87-93%) and high specificity (83-97%) for diagnosing TBP.
Differential Diagnosis:
High ADA : Strongly suggests TBP.
Low ADA : Essentially rules out TBP in a patient with a low pre-test probability, but high levels can rarely be seen in purulent (bacterial) pericarditis or certain malignancies.
0 Comments
0 Shares
188 Views
0 Reviews